:max_bytes(150000):strip_icc()/how-to-heal-a-broken-bone-quickly-2549327-5bb7c3c5c9e77c0051574e48.png) 6 Ideas for Healing Broken Bones as Quickly as Possible
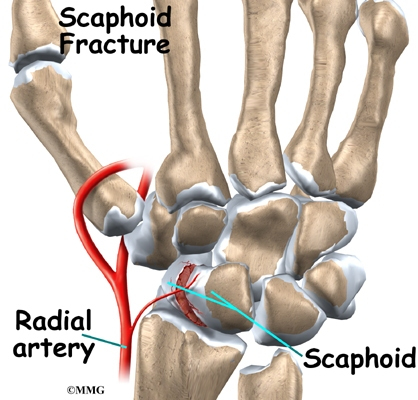
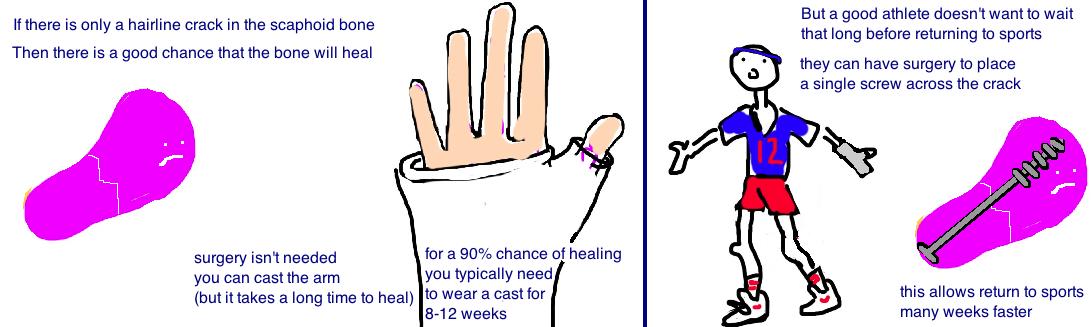
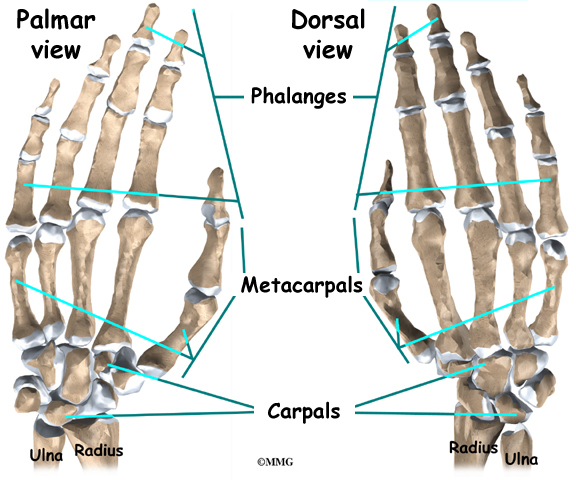
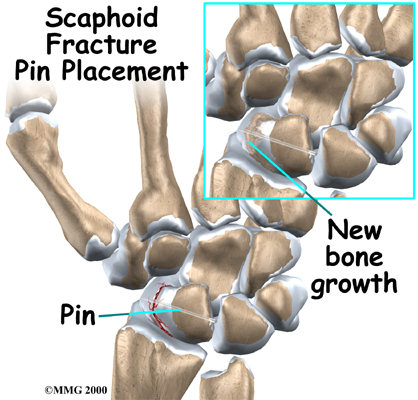
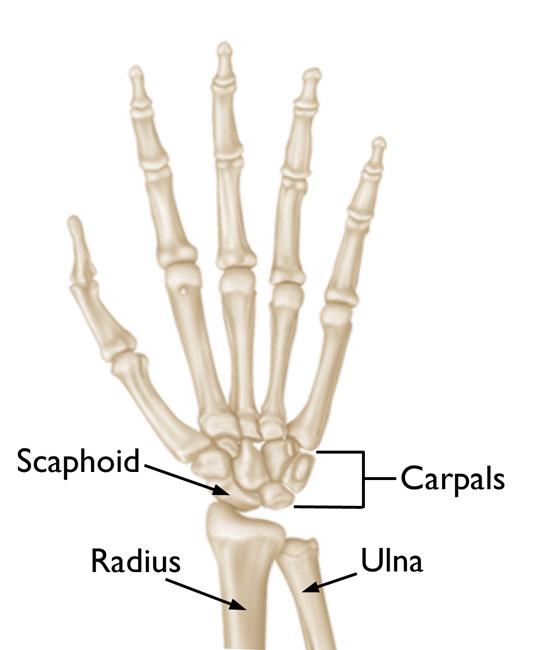
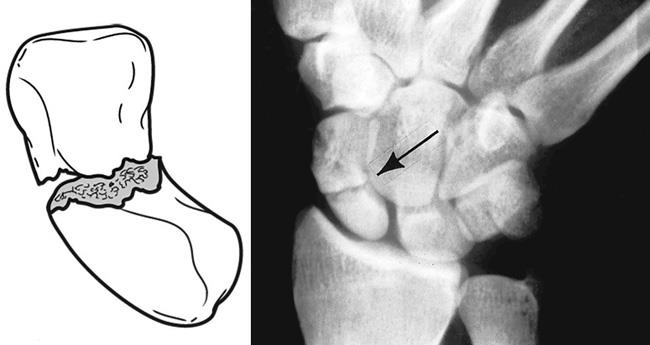
6 Ideas for Healing Broken Bones as Quickly as PossibleNo resultsNo resultsProcessing results.... Treatment of scaphoid lesions and administrationRehabilitation Physical therapyThe general principles for rehabilitation of wrist injuries, including rehabilitation of scaphoid fractures, are as follows: All of these injuries require some type of rehabilitation. [] Specific constraints apply to rehabilitation. Pain is a limiting factor, because it dictates the duration of immobilization and the limits designed to mobilize and strengthen the wrist. Injured wrist eema is present to some degree and may involve the entire upper hand or extremity. The functional disuse itself results in edema. The most important preventive measures are the lifting and active movement of uninjured joints. Modalities (e.g. intermittent compression units from Jobst, massage) can be used later for chronic edema associated with traumatic wrist injuries. The wrist is always stiff after immobilization for more than a few weeks. Mobilization cannot begin until the injured tissue has healed enough to provide some degree of stability. Active wrist ROM exercises should start as soon as the cast is removed. Pronation and supposition should not be overlooked. Mobilizing the joint is desirable before the bone and soft tissues have healed completely. Several fragments are required to protect and support the wrist at its final healing stage. Muscles that cross the wrist should be strengthened after the wrist has healed, the edema has been controlled, and the movement has improved. Functional activities and progressive resistance exercises are used. The flexors of the wrist and the extenders are actively contracted against the maximum resistance through a full arch of motion. Rehabilitation Considerations Immediately After A Week Damage For molten fractures Active range of motion (AROM) and passive range of motion (PROM) to digits, except the thumb, which is immobilizedAROM and active-assisted range of motion exercises (AAROM) to the shoulder Asymmetric exercises to biceps, triceps and muscles deltoids After open-reducing internal fixing surgery (ORIF)Elevation of the arm to treat AROM dependent edema and Dygite PROM, except the AROM and AAROM thumbs to the elbow and shoulder ExercisesIsometrical to the biceps, triceps and muscles deltoideLimitation of supination and pronationRehabilitation considerations in 2 weeks The doctor may obtain omeal scans in case of continuous pain and tenderness in the mailbox with negative radiograph findings. Bone stimulators have increasingly been used for stable and non-displaced fractures and for suspicious scafoid fractures with negative radiographic findings, although both uses remain somewhat controversial. A short plaster is indicated for a suspicious fracture, while a long plaster is used for a known fracture. The patient should continue the ROM exercises for molten fractures and ORIF, as indicated above. Rehabilitation considerations in 4-6 weeks For melted fractures Continue exercises as above. Limit supposition and pronation. Change the long-range plaster to a short-range plaster (called erased indicates stability). After surgery ORIF Advance therapy with mild wrist AROM and mild opposition and bending/extension exercises. Continue the elbow and shoulder exercises. Remove the short cast at 6 weeks if the fracture appears to be cured radiographically. Use a doll tip for protection. Rehabilitation Considerations in 8-12 weeks For melted fractures Remove the short plaster at 10-12 weeks if the fracture appears to be radiographic and clinically cured. A wrist cream can be used to protect For molten and later fractures ORIFConsider pulsed electrical stimulation if there is no evidence of union is observed in 8 weeks, and consider surgery with bone graft if progress is not observed in 12-14 weeks. Advance therapy with soft AROM of the wrist and with thumb exercises. Start strengthening grip with the use of silicone putty at 10 weeks. Advance as tolerated to progressive resistive exercises (PREs). Occupational therapy The patient usually needs retraining in the performance of daily life activities (ADL). The occupational therapist provides the patient with compensatory strategies to use when completing the ADL tasks. Or physical or occupational therapy is necessary to regain strength and ROM on the wrist and hand affected. The guidelines for rehabilitation are discussed earlier in the Physical Therapy section. Medical issues/Complications See the following list: Scaphoid injuries and prolonged casting - These results in lost work days and decreased work efficiency. Notion of scaphoid fracture [, ] This complication is influenced by delayed diagnosis, gross displacement, associated carpus lesions and the supply of damaged blood. Of these fractures, 40% are not diagnosed at the time of the original injury. Nounion is a 20% more common in . [] The incidence of avascular necrosis is approximately 30-40%, which occurs most often in fractures of the proximal third. Scapular dissociation is a known complication of the scaphoid fracture. Surgical interventionIndictions for immediate surgical remission include the following: Displaced or unstable fractures require percutaneous fixing of pins or fixing of compression screws to prevent malunion. The internal fixing is made with Kirschner soft wires or with a Herbert screw. [] A bibliographical review of Dunn et al indicated that scafoid staples fixation is associated with a union rate of 94.7%, with 95.7% of patients returning to work after 9.8 weeks, on average. The complication rate in the study was low (9.0%), with the removal of hardware required in 7.5% of cases. [] Surgery is increasingly used for patients (especially athletes) who will not tolerate prolonged casting. Escafoid nounions are treated in one of the following ways: Due to the significant time required for the binding of proximal post fractures, some surgeons recommend the primary fixing of these fractures even when they do not move. The Matti-Russe procedure involves the treatment of non-displaced fractures by excavating the scafoids and placing a corticocanceloso fly bone graft. If the proximal pole is avascular and there is no significant radiocarpia present, you can try to revascularize the scaphoid bone with a vascularized bone graft of the radio. A review of more than 5000 cases found that the vascularized bone graft (with or without internal fixation) was 91% successful, that the non-vascularized bone graft with internal fixation was 84% successful, and that the non-vascularized bone graft without internal fixation was 80% successful. [] A carpal silicone implant is no longer recommended. Once degenerative arthritis is evident in the radiocarpal joint, the rescue procedures include proximal fila carpectomy, scaphoid excision, and intercarpia wrist arthrodesis or total. In general, consultation with a hand specialist or orthopedic surgeon should be obtained for an open or unstable scaphoid fracture or for a scaphoid fracture that requires fixation. Other Treatments Please see the section of Physical Therapy. Undisplaced fractures Initially, undisplaced fractures are treated with a long arm plaster with the wrist in neutral position for 6 weeks, followed by a short arm cast for 6 additional weeks, until the roentgenographic union is evident. If there is a displacement or extension of the fracture line after 6 weeks, the patient should be referred for surgical evaluation. After immobilization, active ROM exercises to the forearm, wrist and thumb must be performed 6-8 times a day. A static doll with a neutral doll should be used between exercise sessions and at night. Displaced fractures These usually require ORIF using wires and screws. So, a short thumb spica of arms is needed for 8-12 weeks until the roentgenographic union is evident. At 4 months after surgery, the bending and dynamic extension of the wrist can be started. At 6 months, the patient usually resumes normal use of his hand. Electrical stimulation, or pulsed electromagnetic stimulation, has been proposed as beneficial in cases of undisplaced scaphoid notion; however, this technique remains controversial, because no study has been conducted to compare the results of using PES only with those of using only the molten immobilization. Related Medscape Reference theme: Eiff MP, Hatch RL, Petering RC. Carpal fractures. Fracture management for primary care. 3rd edition. Philadelphia: Saunders; 2012. Cheung GC, Lever CJ, Morris AD. X-ray diagnosis of acute scaphoid fractures. J Hand Surg [Br]. 2006 Feb. 31(1):104-9. Toth F, Sebestyen A, Balint L, et al. Doll position for scaphoid X-ray. Eur J Radiol. 2007 Oct. 64(1):126-32. . Beeres FJ, Hogervorst M, Rhemrev SJ, et al. Prospective comparison of suspicious scaphoid fractures: bone scintigraphy versus clinical result. Injuries. 2007 Jul. 38(7):769-74. Beeres FJ, Hogervorst M, den Hollander P, et al. Results of routine bone scintigraphy in suspected scaphoid fractures. Injuries. 2005 Oct 36(10):1233-6. Dias JJ, Dhukaram V, Abhinav A, et al. Clinical and radiological result of the immobilization of foundry versus surgical treatment of acute scaphoid fractures in an average follow-up of 93 months. J Bone Joint Surg Br. 2008 Jul. 90(7):899-905. Seitz WH Jr., Papandrea RF. Fractures and dislocations of the wrist. Bucholz RW, Heckman JD, Eds. Rockwood and Green fractures in adults. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2002. Williams R, Jupiter DC, Maassen NH. The incidence and risk factors of scaphoid fracture associated with the head and neck radial fracture in trauma patients. J Am Acad Orthop Surg Glob Res Rev. 2019 May. 3 (5):e055. . .Carpenter CR, Pines JM, Schuur JD, Muir M, Calfee RP, Raja AS. Fracture of adult scaphoids. Acad Emerg Med. 2014 Feb. 21 (2):101-21. Duckworth AD, Jenkins PJ, Aitken SA, Clement ND, Court-Brown CM, McQueen MM. Epidemiology of the scaphoid fracture. J Trauma. 2011 Oct 13. Hannemann PF, Brouwers L, Dullaert K, et al. Determination of the union of fracture of scaphoid waist by conventional radiographic examination: an analysis of reliability and validity. Arch Orthop Trauma Surg. 2015 Feb. 135(2):291-6. Moller JM, Larsen L, Bovin J, et al. Diagnosis of the magnetic resonance of the fracture of the scaphoid bone: impact of a new practice where the images are read by the radiographs. Acad Radiol. 2004 Jul. 11(7):724-8. Mallee WH, Wang J, Poolman RW, et al. Computed tomography against magnetic resonance against bone scintigraphy for clinically suspicious scaphoid fractures in patients with negative flat X-rays. Cochrane Database Syst Rev. 2015 Jun 5. CD010023. Karantanas A, Dailiana Z, Malizos K. The role of the MR image in scaphoid disorders. Eur Radiol. 2007 Nov. 17(11):2860-71. Jenkins PJ, Slade K, Huntley JS, et al. A comparative analysis of accuracy, diagnostic uncertainty and the cost of imaging patterns in suspicious scaphoid fractures. 2008 Jul. 39(7):768-74. . Tibrewal S, Jayakumar P, Vaidya S, Ang SC. Function of MRI in the diagnosis and management of patients with clinical scaphoid fracture. Int Orthop. 2011 Sep 7. Ng AW, Griffith JF, Taljanovic MS, Li A, Tse WL, Ho PC. Is the magnetic resonance improved by contrast to evaluate the proximal fragmentary vascularity in delayed and non-union scaphoid fracture useful? Skeletal radio. 2013 Jul. 42(7):983-92. . Brooks S, Cicuttini FM, Lim S, Taylor D, Stuckey SL, Wluka AE. Cost effectiveness of adding magnetic resonance imaging to the usual management of suspicious scaphoid fractures. Br J Sports Med. 2005 Feb. 39(2):75-9. Bervian MR, Ribak S, Livani B. Escafóid fracture no union: correlation of radiographic images, evaluation of histological feasibility of proximal fragment and estimation of feasibility in surgery: diagnosis of scafóid pseudarthrosis. Int Orthop. 2015 Jan. 39(1):67-72. . Beeres FJ, Hogervorst M, Rhemrev SJ, et al. Fiability of bone scintigraphy due to suspected scaphoid fractures. Clin Nucl Med. 2007 Nov. 32(11):835-8. . Finkenberg JG, Hoffer E, Kelly C, et al. Diagnosis of scaphoid fractures hidden by intrasonic vibration. J Hand Surg [Am]. 1993 Jan. 18(1):4-7. Brotzman SB, Wilk KE, eds. Orthopedic Rehabilitation Manual. 2nd edition. Philadelphia, Pa: Elsevier; 2007. Cohen MS, Jupiter JB, Fallahi K, Shukla SK. Notion of scaphoid waist with treated humpback deformity without structural bone graft. J Hand Surg Am. 2013 Rev. 38(4):701-5. . Capo JT, Shamian B, Rizzo M. Percutaneous screw fixing without bone grafting of non-scaphoid union. Isr Med Assoc J. 2012 Dec. 14(12):729-32. Dinah AF, Vickers RH. Smoking increases the rate of operation failure for the established non-union of the scaphoid bone. Int Orthop. 2007 Aug. 31(4):503-5. Dunn J, Kusnezov N, Fares A, Mitchell J, Pirela-Cruz M. The Scaphoid Staple: A Systematic Review. Hand (N Y). 2017 May. 12 (3):236-41. Munk B, Larsen CF. Scaphoid notion bone grafting: systematic review of 147 publications, including 5,246 cases of scaphoid notion. Acta Orthop Scand. 2004 Oct. 75(5):618-29. . Scott R Laker, Deputy Professor of MD, Department of Physical Medicine and Rehabilitation, Faculty of Medicine, University of Colorado; Medical Director, Center for Health of Lonely Trees Scott R Laker, MD is a member of the following medical societies: , Disclosure: Nothing to reveal. Dustin Anderson, MD Resident Physician, Department of Physical Medicine and Rehabilitation, University of Colorado School of Medicine Dustin Anderson, MD is a member of the following medical societies: , Disclosure: Nothing to reveal. Francisco Talavera, PharmD, PhD Associate Professor, University of Nebraska Medical Center College of Pharmacy; Chief Editor, Medscape Drug ReferenceDisclosure: Received Medscape's salary for employment. Medscape. Patrick M Foye, MD Director of the Center of Pain Coccyx, Professor of Physical Medicine and Rehabilitation, Rutgers New Jersey Medical School; Co-director of Musculoskeletal Scholarship, Co-director of Back Pain Clinic, University Hospital Patrick M Foye, MD is a member of the following medical societies: Disclosure: Nothing to reveal. Stephen Kishner, MD, Professor of Clinical Medicine, Physics Medicine and Residence Program Residence, Louisiana State University School of Medicine in New Orleans Stephen Kishner, MD, MHA is a member of the following medical societies: , Disclosure: Nothing to reveal. J Michael Wieting, DO, MEd, FAOCPMR, FAAOE Senior Associate Dean, Professor of Physical Medicine and Rehabilitation, Professor of Osteopathic Manipulative Medicine, Lincoln Memorial University-DeBusk College of Osteopathic Medicine J Michael Wieting, DO, MEd, FAOCPMR, FAAOE is a member of the following medical societies: , American Association of Osteopathic Examiners, , , , Gold Humanism Honor Society, International Society for Communication Science and Medicine, Michigan Osteopathic Association, Oklahoma Osteopathic Association, Tennessee Osteopathic Medical Association Disclosure: Nothing to reveal. Robert Irwin, MD Consulting Staff, Florida Orthopaedic Institute Robert Irwin, MD is a member of the following medical societies: , Physical Society of the Thorn, Sports and Occupational Rehabilitation , , Disclosure: Nothing to reveal. Deborah Saint-Phard, MD Associate Professor, Department of Physical Medicine and Rehabilitation, Department of Orthopedic Surgery, University of Colorado School of Medicine; Founder and Director, CU Women's Sports Medicine at UCHealth Deborah Saint-Phard, MD is a member of the following medical societies: , Physical Society of the Thorn, Sports and Occupational Rehabilitation Dissemination: Nothing to reveal. Maria Carmen Espiritu, MD, PT Consulting Staff, Espiritu Clinic, Clinch Valley Medical Center Maria Carmen Espiritu, MD, PT is a member of the following medical societies: and the Dissemination: Nothing to reveal. What do you want to print? Find us aboutMembershipWebMD NetworkEditions
Curation of broken bones as fast as possible 6 Ideas for the healing of the speed bone after damageJonathan Cluett, MD, is an orthopedic surgeon certified by the board with training of subspecialty in sports medicine and arthroscopic surgery. Grant Hughes, MD, is a rheumatologist certified by the board. He is an associate professor at the University of Washington School of Medicine and head of rheumatology at the Portview Medical Center in Seattle. Fractures, broken bones – you can call it what you want, are one of the most common orthopedic problems; about 7.9 million broken bones come to medical care every year in the United States. Despite what you've heard, a broken bone is no worse than a fracture: both mean the same. In fact, the word fracture, according to the Oxford English Dictionary, is defined as "the act of being broken." There are different types of fractures and broken bones, but these words are one and the same and can be caused in various ways. And, although the healing process seems slow, there are several factors that you can focus on to make sure you give you the chance of the best recovery possible. How fractures are hidden Fractures occur because a bone area is not able to withstand the energy put on it (very obvious, but becomes more complicated). Therefore, there are two critical factors to determine why a fracture occurs: the energy of the event and the strength of the bone. The energy can be sudden, high-energy (e.g. car accident), or chronic, low energy (e.g.) He can be normal or decrease (for example, the weak bone is seen in patients with ). A very simple problem, the broken bone, became much more complicated! Thus, fractures are more often caused by a force such as a car accident or a drop in height, or by abnormally weak bones like those of older people with osteoporosis. The reason the fracture occurred is often useful to determine the best treatment for the injury. Most common broken bones treat fractures along the skeletal frame, except the skull (neurocirujane) and the face (ENT, ear, nose and throat of the surgeon). Extrusion fractures are more common, and usually occur in men under 45 years of age, and then become more common in women over 45 years of age. After this age, women have a faster loss of bone density and a probability of developing bone thinning. That is why women are particularly susceptible to osteoporosis and subsequent fractures. The most common fracture before the age of 75 is a . In those over 75 years, become the most common broken bone. Curative broken bones The healing of a broken bone takes time, and depends on several factors such as the age of the patient, general health, nutrition, blood flow to the bone and treatment. Following these six tips you can help: Everyone wants his bone to heal as quickly as possible, but the truth is that he will still need time for the injury to recover. Taking these steps will ensure that you are doing everything you can to make your bone recover as soon as possible. Role of medicines If you have sustained a broken bone, make sure your doctor is aware of the medications you are taking. There are some medicines that can interfere with fracture healing, and he should be discussed with your doctor. In some situations, your doctor may recommend that specific medicines be left tuned after a fracture to allow bone healing. A type of medication that some doctors believe may delay the fracture by healing our nonsteroidal anti-inflammatory drugs (NSAIDs), such as Motrin or Aleve. NSAIDs have been shown in animal models to delay the healing of fractures. Usually, studies have found that healing is delayed when the medication is given at very high doses, much higher than a typical patient would take. Having said this, in fractures that are particularly difficult to cure, your doctor may recommend avoiding these medications. Just as there are medicines that can delay fracture healing, there are also some medicines that can help accelerate fracture healing. These medicines include . People who have difficulty healing fractures may want to discuss with your doctor if they should take specific types of medications to help with fracture healing. A word from Muywell Keeping a broken bone can be a frustrating experience. Expecting the fracture to cure can be even a more frustrating experience. Fortunately, there are steps that can be taken to ensure that the fracture is healthy as quickly as possible. Most of the time, the steps of the common sense to take good care of your body will allow a quick and effective healing of the fracture. In some situations, your doctor may help advise you on some additional steps that can help accelerate healing. Dealing with joint pain can cause major disruptions to your day. Sign up and learn how to better care for your body. Click below and click send! Thank you, for signing. There was a mistake. Please try again. Buza JA, Einhorn T. Clin Cases Miner Bone Metab. 2016;13(2):101-105. doi:10.11138/ccmbm/2016.13.2.101 Hernández CJ, Van der meulen MC. J Bone Miner Res. 2017;32(6):1157-1162. doi:10.1002/jbmr.3078 Hunter DJ, Sambrook PN. Arthritis Res. 2000;2(6):441-5. doi:10.1186/ar125 Karl JW, Olson PR, Rosenwasser MP. J Orthop Trauma. 2015;29(8):e242-4. doi:10.1097/BOT.0000000000000312Tomlinson RE, Silva MJ. Bone Res. 2013;1(4):311-22. doi:10.4248/BR201304002 Karpouzos A, Diamantis E, Farmaki P, Savvanis S, Troupis T. J Osteoporos. 2017;2017:4218472 doi:10.1155/2017/4218472Bowes J, Buckley R. World J Orthop. 2016;7(12):793-800. doi:10.5312/wjo.v7.i12.793 Ebrahim S, Mollon B, Bance S, Busse JW, Bhandari M. Can J Surg. 2014;57(3):E105-18. doi:10.1503/cjs.010113 Geusens P, Emans PJ, De jong Jheumarol 2013;25(4):524-31. doi:10.1097/BOR.0b013e32836200b8 Hegde V, Jo JE, Andreopoulou P, Lane JM. Osteoporos Int. 2016;27(3):861-871. doi:10.1007/s00198-015-3331-7Bishop JA, Palanca AA, Bellino MJ, Lowenberg DW. "" J Am Acad Orthop Surg. 2012 May;20(5):273-82.Hak DJ, et al. "" Injuries. 2014 Jun;45 Suppl 2:S3-7. Thank you, for signing. There was a mistake. Please try again.
Scaphoid Fracture Surgery | Diagnosis, procedure & recovery | SportsMD
Examination and treatment of scaphoid fractures and pseudarthrosis | Tidsskrift for Den norske legeforening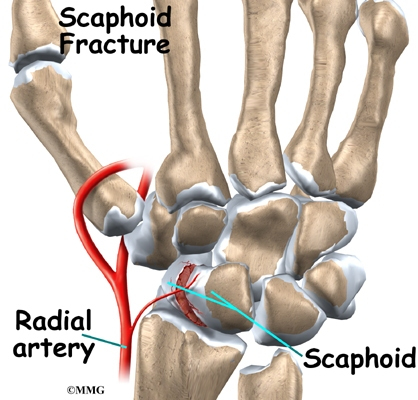
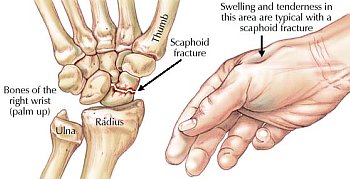
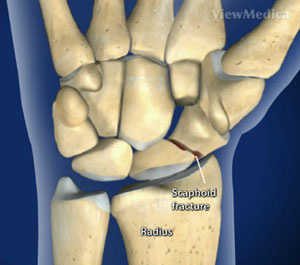
Scaphoid Fracture of the Wrist | eOrthopod.com
Article on: Scaphoid fractures | Standard of Care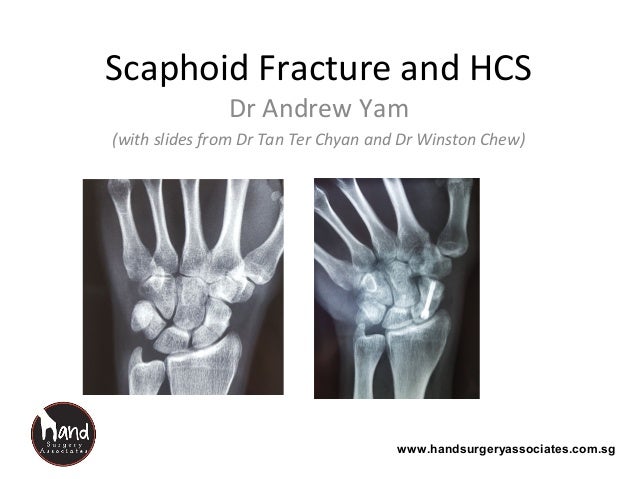
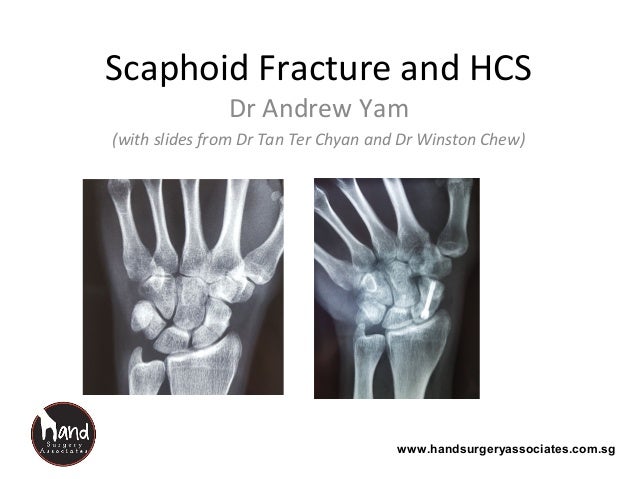
Scaphoid fracture and hcs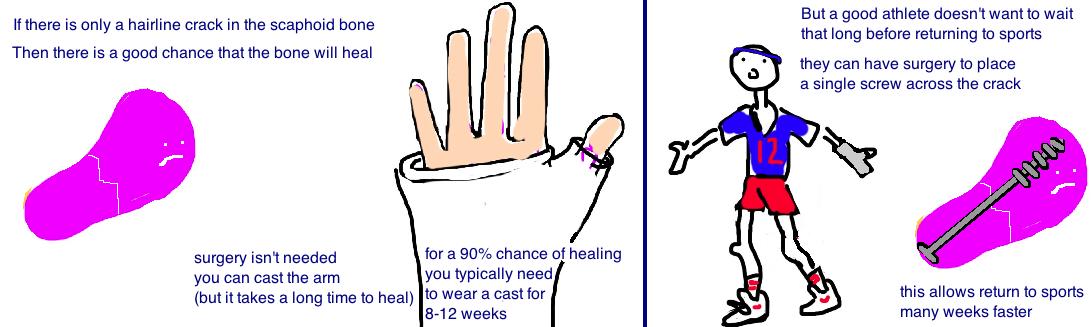
Scaphoid Fracture — Bone Talks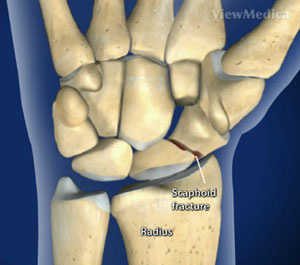
Scaphoid Fracture
Mr Paul Jarrett | Scaphoid Fractures | Murdoch Orthopaedic Clinic/wrst1-56a6d91d5f9b58b7d0e51955.jpg)
Scaphoid Fracture: Causes, Symptoms, Diagnosis, and Treatment
Scaphoid Fracture: All About This Common Wrist Injury and Treatment
Scaphoid Fracture - Hand - Orthobullets
Scaphoid fractures treated with a volar percutaneous approach. Analysis and results in 92 cases | Revista Española de Cirugía Ortopédica y Traumatología (English Edition)
Scaphoid Fracture | Treatment | No Referral Needed | Action Rehab
Scaphoid Fracture|Types|Causes|Symptoms|Treatment|Physical Therapy|
Scaphoid fracture - Wikipedia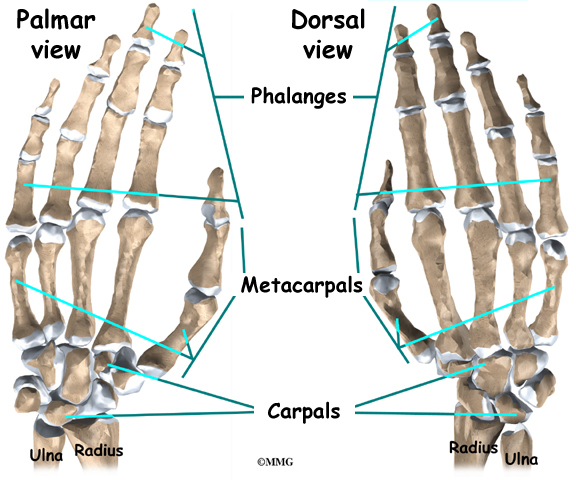
Scaphoid Fracture of the Wrist | eOrthopod.com
Scaphoid Fractures and Nonunion: Wrist Fractures and Treatment
Scaphoid Fracture | FAQs Answered | Dr. Seeds Blog
Navicular Fracture in Foot and Wrist
Scaphoid Fracture Treatment - Heal faster without a cast - YouTube
Scaphoid Fracture in the Elite Athlete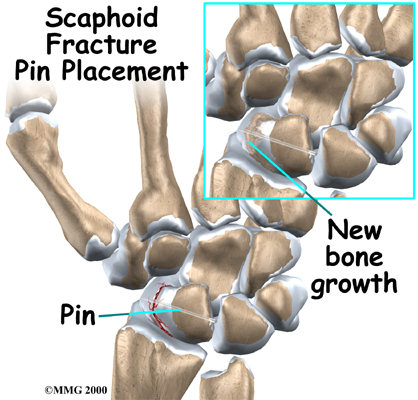
Physical Therapy in Colorado Springs for Wrist Pain - Scaphoid Fracture
Scaphoid Fracture - an overview | ScienceDirect Topics
13 Volar Percutaneous Scaphoid Screw Fixation | Musculoskeletal Key
Examination and treatment of scaphoid fractures and pseudarthrosis | Tidsskrift for Den norske legeforening
Scaphoid Fracture in the Elite Athlete
Hairline Wrist Fracture
How to Speed up Your Recovery from a Scaphoid Fracture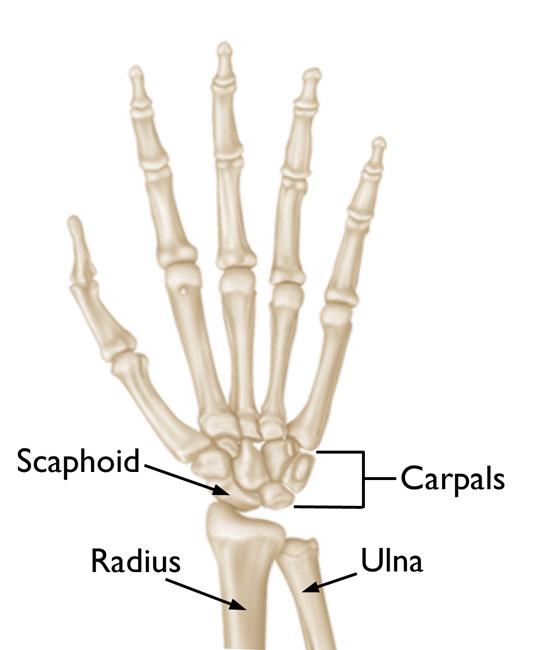
Scaphoid Fracture of the Wrist - OrthoInfo - AAOS
Scaphoid Fractures
Broken or Sprained Wrist - Brandon P. Donnelly, MD
Scaphoid Fracture - Hand - Orthobullets
Scaphoid Fracture - an overview | ScienceDirect Topics
A 24-year-old patient with a proximal pole fracture (scaphoid fracture... | Download Scientific Diagram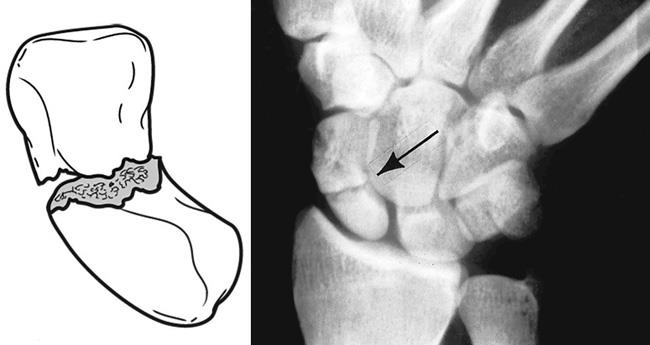
Scaphoid Fracture of the Wrist - OrthoInfo - AAOS
Scaphoid Fracture and Avascular Necrosis | SpringerLink
Scaphoid Fracture - Physiopedia
Scaphoid Fractures: How They Happen, Signs You Have One, and How To Treat It | STACK
Alex Gordon Scaphoid Fracture – Kenneth P. Unruh, M.D. of Orthopaedics and Sports Medicine Consultants, LLC
Scaphoid Fractures: How They Happen, Signs You Have One, and How To Treat It | STACK
:max_bytes(150000):strip_icc()/how-to-heal-a-broken-bone-quickly-2549327-5bb7c3c5c9e77c0051574e48.png) 6 Ideas for Healing Broken Bones as Quickly as Possible
6 Ideas for Healing Broken Bones as Quickly as Possible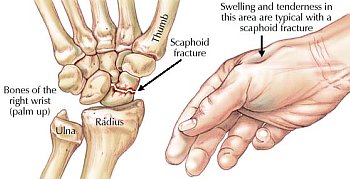


/wrst1-56a6d91d5f9b58b7d0e51955.jpg)






















Posting Komentar untuk "how to heal scaphoid fracture faster"